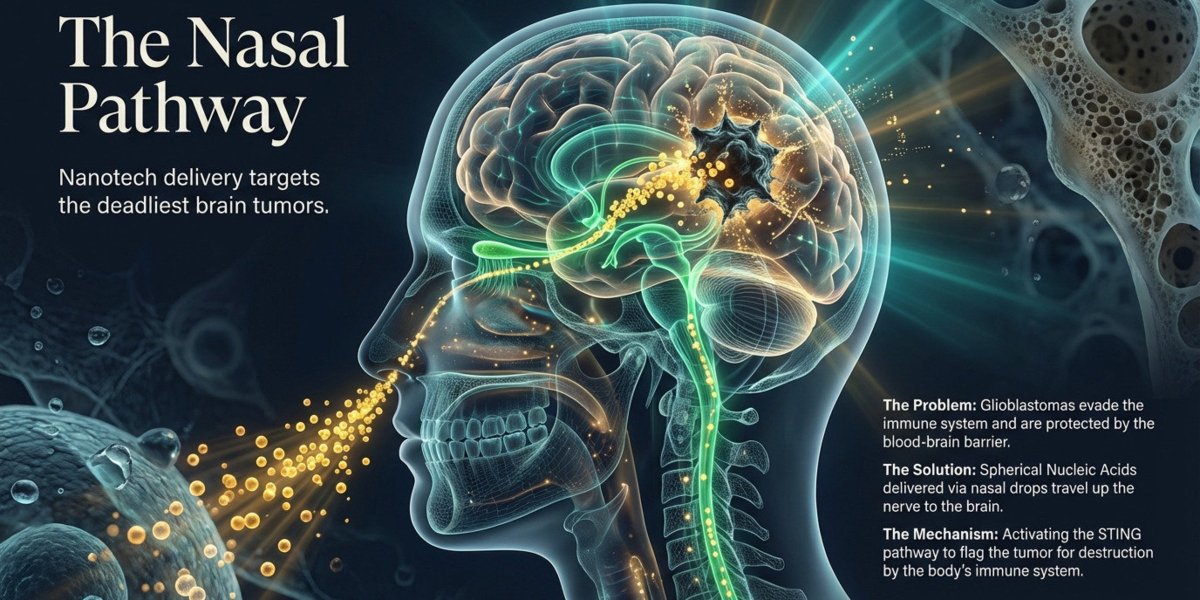
Solid tumors have a cruel irony built into them. They’re often packed with immune cells that should be attacking the cancer—but instead, these cells sit dormant, suppressed by the very tumor environment they’re trapped within. Tumors contain immune cells called macrophages that are naturally capable of attacking cancer, however the tumor environment suppresses these cells, preventing them from doing their job.
Now researchers at the Korea Advanced Institute of Science and Technology (KAIST) have found a way to flip the script entirely: transforming these sleeping sentinels into active cancer killers without ever removing them from the body.
The Challenge with Solid Tumors
Solid tumors including gastric, lung, and liver cancers form dense structures that block immune cells from entering or functioning effectively. This physical and biological fortress is why many promising immunotherapies that work brilliantly against blood cancers struggle when confronted with these compact masses.
Enter CAR-macrophages—chimeric antigen receptor-equipped immune cells that represent a promising next step in cancer treatment. These cells can directly engulf cancer cells and also stimulate nearby immune cells, helping to strengthen and expand the body’s overall anticancer response.
But there’s been a problem: traditional CAR-macrophage therapies rely on extracting immune cells from a patient’s blood, growing them in the laboratory, and genetically modifying them before returning them to the body—a process that is expensive, time-consuming, and difficult to apply widely in real-world clinical settings.
Reprogramming Cells Where They Live
The KAIST team, led by Professor Ji-Ho Park from the Department of Bio and Brain Engineering, took a radically different approach. Rather than extracting cells, they focused on the tumor-associated macrophages already gathered around the tumor site.
Their approach uses lipid nanoparticles engineered to be easily taken up by macrophages loaded with both mRNA that carries cancer-recognition instructions and an immune-activating compound. When injected directly into the tumor, these nanoparticles are absorbed by local macrophages like a molecular Trojan horse.
The result? This method creates CAR-macrophages by directly converting the body’s own macrophages into anticancer cell therapies inside the body.
Remarkable Results
When the treatment was injected into tumors, macrophages quickly absorbed the nanoparticles and began producing proteins that identify cancer cells while immune signaling was activated. The newly formed enhanced CAR-macrophages demonstrated dramatically improved cancer-killing ability and stimulated surrounding immune cells, creating a cascading anticancer response.
In animal studies using melanoma—the most aggressive form of skin cancer—the results were striking. Tumor growth was significantly suppressed, and the therapeutic effect was shown to have the potential to extend beyond the local tumor site to induce systemic immune responses. This suggests the approach might help combat metastatic cancers, where cancer has spread beyond the original tumor.
A New Paradigm
Professor Park emphasized the significance: the study presents a new concept that generates anticancer immune cells directly inside the patient’s body while simultaneously overcoming key limitations of existing CAR-macrophage therapies—delivery efficiency and the immunosuppressive tumor environment.
The implications extend beyond the science. By eliminating the need for complex laboratory cell extraction and modification, this approach could dramatically reduce costs and make advanced immunotherapy accessible to far more patients. No cleanroom facilities. No weeks of waiting. Just a direct injection that turns the tumor’s own suppressed defenders into an attacking force.
The research, published in ACS Nano, represents a fundamental shift in how we think about cancer immunotherapy—not as something we build outside the body and introduce, but as a capability we can unlock within the battlefield itself.
This topic was featured in Great News podcast episode 28
Source: SciTechDaily