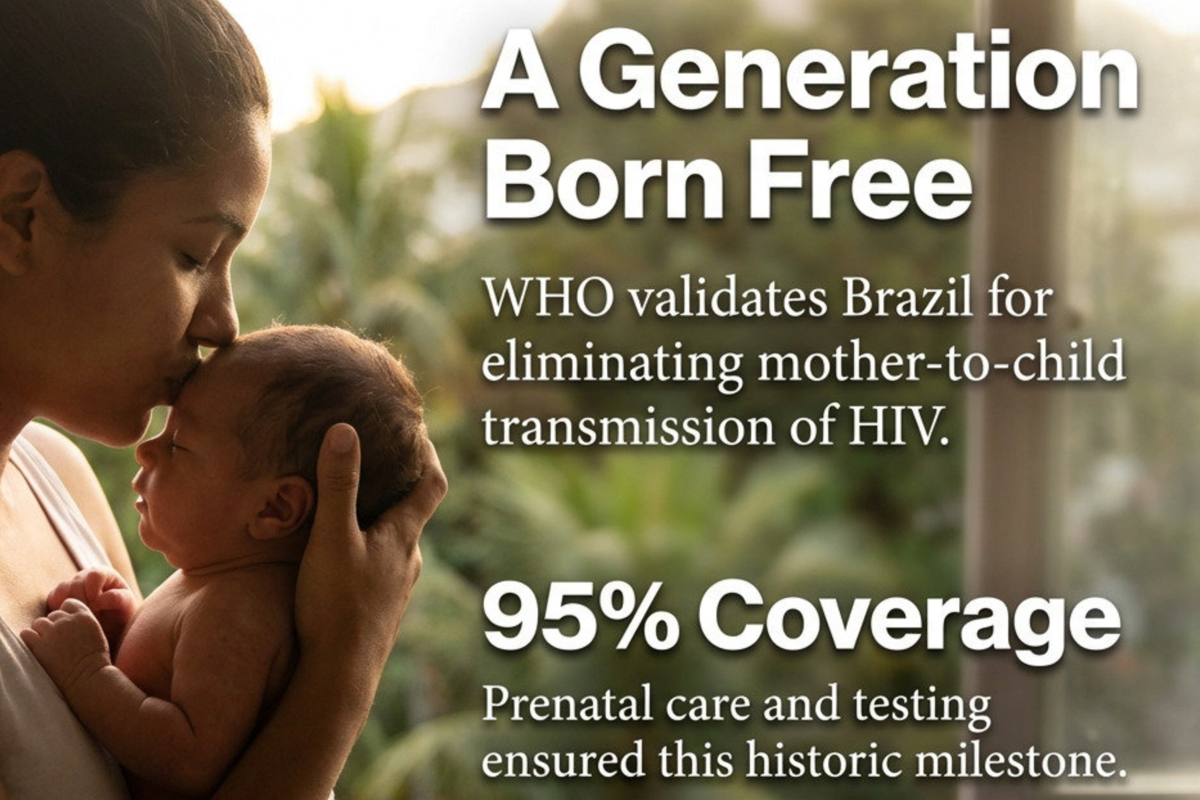
Elimination of Mother-to-Child HIV Transmission in Brazil
The World Health Organization (WHO) has officially validated Brazil for the elimination of mother-to-child transmission (EMTCT) of HIV. This milestone is particularly significant as Brazil is the first country with a population exceeding 100 million to reach this status.
- Validation Criteria: Brazil reduced vertical transmission to below 2% and achieved over 95% coverage for prenatal care, routine testing, and timely treatment.
- Systemic Factors: Success is attributed to the Unified Health System (SUS), which provides universal and free access to health services, and a commitment to breaking monopolies to secure affordable medicines.
- Regional Context: Brazil is the 19th country globally and the 12th in the Americas to achieve this validation.
This story was featured in Great News podcast episode 25

The Great News Podcast is your source for positive news, inspiring stories, and good news from around the world. We skip the doom and gloom of mainstream media to focus on scientific breakthroughs, environmental wins, and the inspiring news that proves the world is getting better. Join Andrew McGivern for a dose of optimism and uplifting stories that will change your perspective on human progress.
It is easy to find the
Keep looking for the good in the world, because it is not only there – its everywhere.
Today, we’re diving into some truly groundbreaking advancements in medicine, environmental protection, and global justice. What if we could ensure every child is born free of a life-altering virus? That is our lead story today. Plus, we have a gene therapy that restores hearing, internet cables that can sense earthquakes, and a new way to store energy using a fluid that looks like a giant protein shake. And don’t forget to stick around for the speed round, where we’ll dive into even more great news

What This Achievement Means
Brazil’s elimination of mother-to-child HIV transmission represents a profound convergence of public health infrastructure, political will, and health equity. Let me unpack the deeper significance:
A Victory Against Biological Inevitability Without intervention, HIV transmission from mother to child occurs in 15-45% of cases. Brazil has reduced this to below 2%—transforming what was once a near-certainty into a preventable tragedy. This isn’t just a statistical achievement; it represents thousands of children who will live HIV-free lives, breaking intergenerational cycles of disease and stigma.
Proof That Universal Healthcare Works at Scale Brazil’s success demolishes the argument that universal healthcare systems can’t deliver specialized interventions effectively in large, diverse populations. The SUS model demonstrates that free, universal access isn’t a luxury—it’s the foundation for eliminating health disparities. Every pregnant woman, regardless of income or geography, receives prenatal care, testing, and antiretroviral treatment. This isn’t charity; it’s infrastructure.
The Power of Pharmaceutical Sovereignty Brazil’s willingness to challenge pharmaceutical monopolies and produce generic antiretrovirals domestically is arguably as important as the clinical protocols themselves. By refusing to accept artificially inflated drug prices, Brazil made treatment financially sustainable at a population level. This is a replicable political strategy that other nations—particularly those in the Global South—can adopt.
How the World Improves When We Work on Problems Like This
1. Health Gains Compound Across Generations When children aren’t born with HIV, they have better educational outcomes, economic productivity, and health trajectories. Their mothers are healthier and can care for families more effectively. These benefits ripple outward—one eliminated transmission prevents decades of medical costs, social support needs, and human suffering.
2. Systems Strengthen Beyond the Initial Target The infrastructure Brazil built—prenatal care networks, testing protocols, treatment distribution systems—doesn’t only benefit HIV prevention. These same systems improve outcomes for detecting gestational diabetes, preventing preterm births, reducing maternal mortality, and catching other infectious diseases early. Solving one problem builds capacity to solve many others.
3. Evidence Shifts Global Norms When a country of 215 million people proves something is possible, it changes what the international community considers achievable. Brazil’s success will influence WHO guidelines, development funding priorities, and policy debates in dozens of countries. It transforms EMTCT from an aspirational goal to an expected standard of care.
4. Health Equity Becomes Measurable Brazil’s achievement required reaching marginalized populations—Indigenous communities in the Amazon, favela residents in urban centers, rural populations far from major hospitals. The validation criteria force countries to confront disparities rather than hide behind national averages. When you must achieve 95% coverage, you can’t ignore the hardest-to-reach 5%.
Critical Lessons for Global Health
Integration Over Verticalization Brazil succeeded by integrating HIV prevention into routine prenatal care rather than creating parallel, disease-specific programs. This approach is more sustainable, less stigmatizing, and more efficient. It suggests that global health initiatives should embed interventions into existing universal health systems rather than creating fragmented vertical programs.
Medicine as a Public Good The decision to challenge pharmaceutical patents and produce generic drugs domestically treats medicines as public health infrastructure, not market commodities. This philosophical stance—that certain goods are too important for profit maximization—could be applied to vaccines, antibiotics, cancer treatments, and other essential medicines.
Trust Requires Consistency High uptake of testing and treatment requires communities to trust the health system. Brazil built this trust through decades of providing free, stigma-free care. This can’t be rushed or manufactured through awareness campaigns alone—it requires institutional reliability over time.
What Still Needs Improvement
Even as we celebrate Brazil’s achievement, we should recognize ongoing challenges:
- Sustainability under political shifts: Universal healthcare systems are vulnerable to budget cuts and political ideology changes
- Indigenous and remote communities: While coverage is high overall, maintaining services in the Amazon and other remote areas remains resource-intensive
- Adolescent and adult HIV prevention: Eliminating vertical transmission doesn’t address new adult infections, which require different interventions
- Regional inequality: Brazil succeeded nationally, but other countries in Latin America and globally still struggle
The Broader Imperative
Brazil’s achievement illuminates a fundamental truth: most “intractable” global health problems are actually political and economic problems. We have the biomedical tools to eliminate mother-to-child HIV transmission everywhere. What varies is the presence of universal health systems, affordable medicines, and political commitment to equity.
When we work on problems like this, we’re not just solving discrete medical challenges—we’re building proof that a different kind of world is possible. One where health isn’t rationed by market logic, where preventing suffering is treated as a collective responsibility, and where we measure success by whether we’ve reached the most marginalized, not just the average.
The question isn’t whether other countries can replicate Brazil’s success. The question is whether they’ll choose to.